Incentive Programs
How to discharge patients - the new process
As we shared in early November, our online patient discharge tool is getting an update. On January 8, the tool was moved to the Member Inquiry section of prism, from Patient Profile.
Any patient discharges submitted through Patient Profile on or after January 8 won’t be processed.
This change comes as Patient Profile is set to be removed from prism on February 1 as part of our Digital First data strategy.
Get more information and step-by-step instructions for the new patient discharge process in our Provider Manual. We’ll also cover the process at our February 8 Virtual Office Advisory (VOA) webinar.
2023 PIP supplemental data audit lists will be sent by Jan. 18
Ensuring the accuracy and integrity of our PCP Incentive Program (PIP) is of the utmost importance to us. To achieve this, we conduct an annual audit of supplemental data provided through Patient Profile and Report 70.
The ACNs required to participate in our 2023 PIP program supplemental data audit have been identified. These ACNs will receive a secure email from their Provider Strategy & Solutions Consultant by Jan. 18 with the requested medical records. This email will appear in prism.
If your ACN was selected, you must respond with the requested medical records by Feb. 1. Failure to do so will result in a 50% penalty for the PIP payout for the program year.
Keep an eye out for an email in prism from our Provider Strategy & Solutions team.
Reminder: 2023 PIP supplemental data and claims deadlines are coming up
As a reminder, we wanted to share with you the following 2023 PIP program deadlines coming up soon:
- Jan. 31, 2024 – Supplemental data submission deadline for Patient Profile, Report 70, MiHIN and HL7. Files submitted after this date won’t be in year-end settlement.
- Feb. 28, 2024 – Claims submission and adjudication deadline. All 2023 claims must be billed and adjudicated by the Priority Health system by this date.
For more information, see the 2023 PIP manual (login required).
There’s still time to register for our upcoming Disease Burden Management program webinar
Have you registered for our Disease Burden Management program webinar?
This webinar contains valuable information on our new Disease Burden Management (DBM) program including ACN eligibility, program requirements, earning incentives and more. We’ll also have a chat feature available to all attendees so you can ask questions and share your feedback.
What is the DBM program?
The Disease Burden Management program replaced our Advanced Health Assessment (AHA) and Persistency programs, which retired on Dec. 31, 2023.
Can’t make it? All webinars are recorded and available on-demand after the presentation, so you can watch at your convenience.
January’s PRA attestation is underway
Our first monthly Provider Roster Application (PRA) cycle of 2024 is currently underway. Attestation for February 2024 PCP rosters will close on Jan. 16, 2024.
Monthly PRA attestation continues
ACNs participating any of the following programs must attest to their PCP rosters monthly:
- PCP Incentive Program (PIP)
- Alternative Payment Models (APM)
- Disease Burden Management program (DBP)
2024 PRA attestation calendar
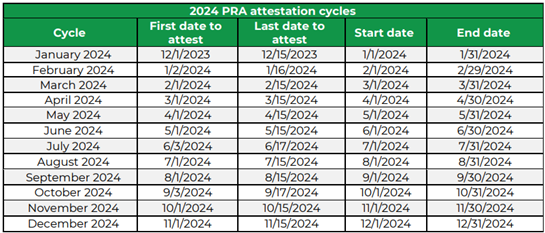
Mark your calendars for the following 2024 PRA attestation dates:
Learn more
Get more information about PRA and how to use the tool in our PRA manual (login required).
Billing and payment
Aligning “assistant at surgery” reimbursement rates with industry standard in March
Providing our members, your patients, the right care at the right cost is one of our top priorities as a nonprofit health plan. As we strive to meet this goal, we occasionally identify opportunities to better align our payment strategies with industry standards.
In March, we’ll align our “assistant at surgery” percent reimbursement rate with the Centers of Medicare and Medicaid Services (CMS) standard as follows:
Commercial & Medicare:
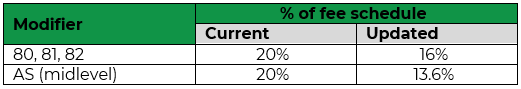
Medicaid:
There will be no change for Medicaid as our percent reimbursement is already aligned with industry standard.
Authorizations
Reminder: PSODs required for procedures and services that may not be covered by Medicare
Pre-service organization determinations (PSODs) are requests used to determine whether an item or service will be covered for a Medicare member.
The PSOD process is like the Traditional Medicare Advanced Beneficiary Notice (ABN) process, protecting all parties involved – the member, provider and Priority Health.
Ensure services not covered, but chosen by the member, don’t become provider liability
When the requested service is covered, we’ll provide the required confirmation. When it’s not covered, we’ll send the Notice of Denial of Medicare Coverage (CMS-10003) to the provider and member. This notice lets the member know they’ll be liable for the cost if they pursue the service.
Bill with modifier GA if the Medicare member decides to move forward with the service knowing coverage has been denied. This will make sure the balance goes to member liability rather than provider liability.
The member, their representative or their provider have the right to request a PSOD. Find out how in our Provider Manual.